Parkinson’s Disease (PD) is a slowly progressive neurodegenerative disorder which mainly affects dopamine-producing neurons in the area of the brain, known as substantia nigra. According to the Parkinson’s Foundation, more than 10 million people worldwide are living with PD. Multiple System Atrophy (MSA), also a neurodegenerative disorder, is on the other hand, a more rare condition which causes gradual damage to nerve cells in the brain. The main type of brain cell affected in MSA are oligodendrocytes, a type of glia involved in maintaining homeostasis, forming myelin and providing support for neurons. MSA evolves quickly and is typically lethal within 10 years after diagnosis.
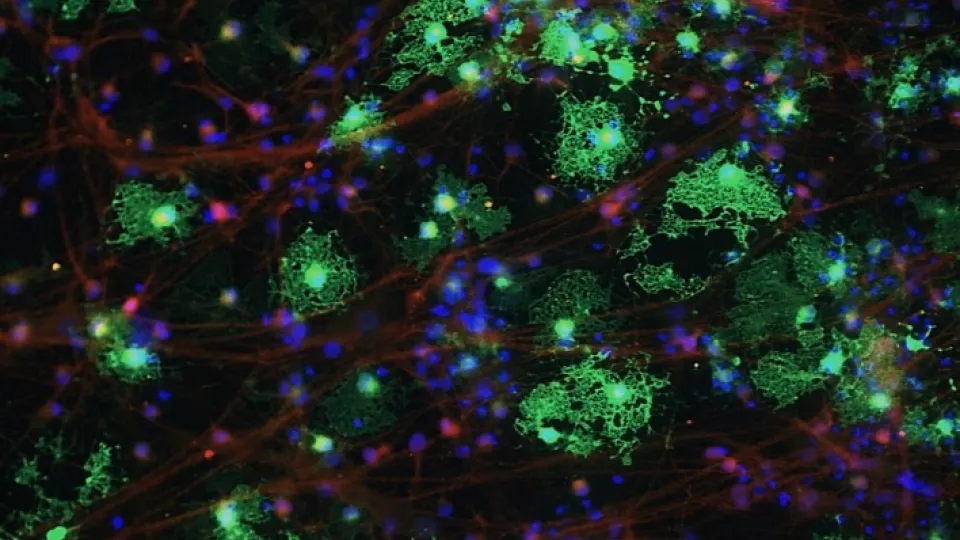
In their latest study, recently published in PNAS, researchers from the Stem Cell Laboratory for CNS Disease Modeling focused their attention on a very aggressive familial form of PD, known as the A53T variant, in addition to MSA. This led them to their latest discovery which demonstrates early cellular pathways and network alterations in patient-induced pluripotent stem cells (iPSCs) - derived oligodendrocytes, from patients with PD and MSA.
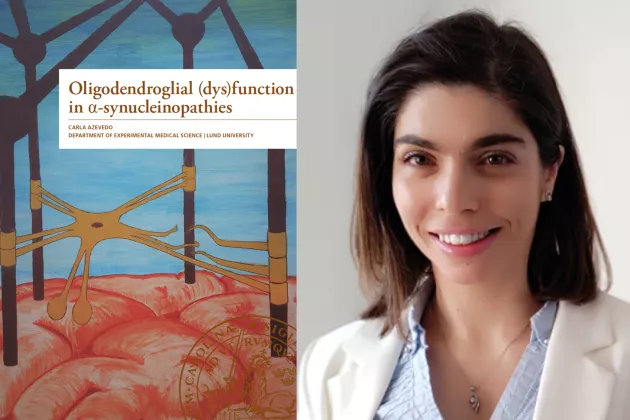
“This work builds on our previous studies where, we demonstrated that oligodendrocytes, like neurons, expressed the SNCA gene encoding for alpha-synuclein (a-syn),” explained Dr. Carla Azevedo, the first author of the study.
This initial discovery revealed the importance of oligodendrocytes in the expression of a-syn, a protein that is abundant in the brain. Based on this, researchers then began asking questions regarding the function of these cells and whether they behaved similarly to neurons that also express this protein, and which become dysfunctional in diseases such as PD. “We hypothesized that if neurons expressing the A53T variant were injured, oligodendrocytes with the same genetic background should also show cellular dysfunction, and contribute to disease progression,” noted Carla.
With a vast library of iPSCs at their fingertips, researchers took iPSCs collected from patients with PD, PD with the A53T variant, and MSA, and employed advanced techniques to compare them to healthy controls.
“The lab has one of the largest libraries of iPSCs in the world, with approximately 500 iPSC lines generated from over 100 patients diagnosed with either Parkinson’s disease, Alzheimer’s disease, Huntington’s disease or amyotrophic lateral sclerosis,” remarked Carla.
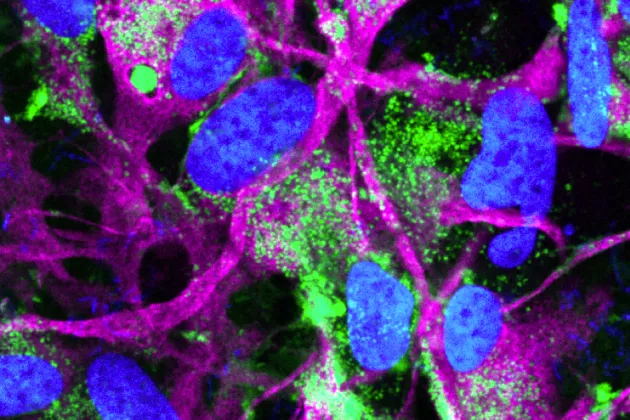
Doing so allowed them to see what was really happening to this specific category of brain cell and revealed that these cells exhibited alpha-synuclein-induced changes in maturation and immune reactive properties. “One of the first things I noticed when looking in the petri dish, was that the cells did not develop, they did not mature,” said Carla.
Using a true population of oligodendrocytes, she was able to confirm that delayed maturation was occurring at both the transcriptomic and protein level. Moreover, she noted that the proteins related to maturation and the differentiation of the cells, were downregulated – meaning that the oligodendrocytes were behind in their differentiation towards myelinating cells.
Even more surprising was the involvement of an immune component triggered by the a-syn protein. “Basically, oligodendrocytes derived from MSA and familial PD became immune reactive instead of pursuing a myelination function. These cells were involved in an immune reaction, resulting in a decreased expression of their differentiation genes. Essentially, they changed their known cell fate,” concluded Carla.
These findings could be used to guide the way towards developing novel therapeutic approaches in the future, for neurodegenerative diseases like PD and MSA, a life-threatening disease currently without a cure.
This study was funded by Swedish foundations such as the Holger Crafoord Foundation, the Shaking Generation Foundation, the Petrus and Augusta Hedlunds Foundation, the Åke Wibergs Foundation, the Greta och Johan Kocks Foundation, as well as donations for science, medicine, and technology at Fysiografen in Lund. The Swedish Research Council, Brainstem–Stem Cell Center for Excellence in Neurology funded by the Innovation Fund Denmark, and the Olav Thon Foundation in Norway, also provided research funding for this study.
Brain samples were obtained in collaboration with The Netherlands Brain Bank, The Portuguese Brain Bank, and The New York Brain Bank at Columbia University. This study was conducted in collaboration with researchers from Lund University including Dr. Oxana Klementieva, and Linköping University.