The brain is a complex organ composed of billions of neurons, whose proper function is dependent on a supportive cell type known as glia. These cells perform a number of functions, including providing neurons with protection, helping the brain to heal following injury, and - in the case of a specific subtype known as astrocytes - supplying neurons with the signals necessary for their growth, development, and survival.
Parkinson’s disease (PD) is characterized by the progressive loss of dopaminergic neurons within the brain, along with the gradual accumulation of the toxic protein alpha-synuclein - forming long filaments known as fibrils. However, little is currently known about the relationship between the accumulation of these protein aggregates, their effect on glial cells and how this impacts the neuronal injury in this brain disorder. A collaborative study between stem cell researchers, neurobiologists and bioinformaticians at Lund University has aimed to shed light on this.
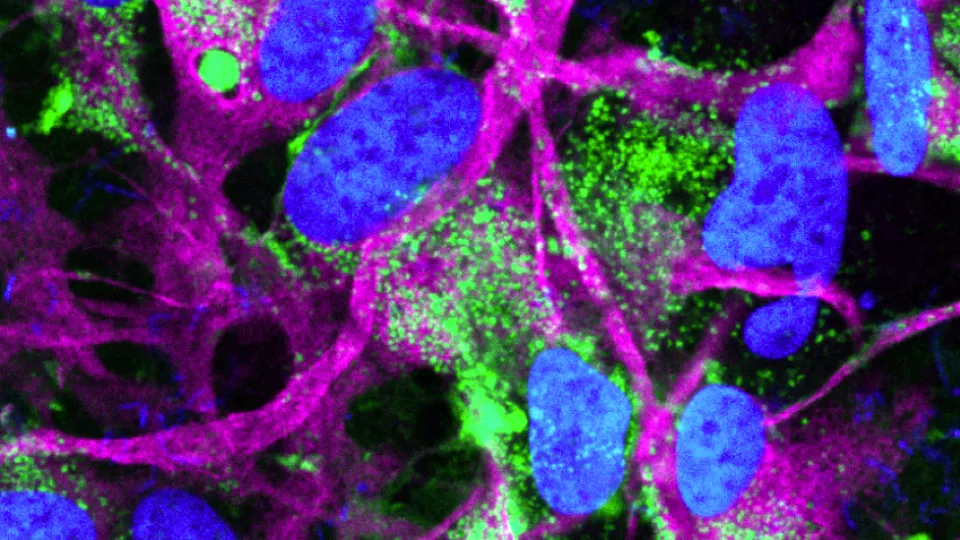
“Due to the lack of availability of human brain samples, we developed protocols for generating astrocytes to study in the lab,” explains Dr. Kaspar Russ, first author of the study. “This was achieved by differentiating pluripotent stem cells, reprogrammed from skin biopsy samples taken from both healthy individuals and PD patients.”
The research team asked how these astrocytes respond to stimulation by either fibrils or the inflammatory factor TNF-alpha, both strongly implicated in the progression of PD. “Strikingly, we identified that astrocytes have different responses to these two types of stimulation,” explains Dr. Russ.
Upon encountering fibrils, astrocytes become antigen-presenting – a process in which the fibrils are digested into smaller fragments, which are then transported to the cell surface to be recognized by the immune system. In contrast, astrocytes treated with TNF-alpha became proinflammatory and start secreting inflammatory factors. If these signals are present together – as is the case in PD – they appear to antagonize each other. This results in astrocytes losing their full ability to become either antigen-presenting or release proinflammatory cytokines.
The researchers also identified that the astrocyte responses were accompanied by an impaired energy production through mitochondrial respiration, more severe in PD astrocytes compared to healthy cells. On top of this, they also observed that PD astrocytes reacted against high quantities of monomeric synuclein - something that healthy astrocytes have no problem with - instead releasing inflammatory factors including TNF-alpha.
“Our findings suggest that exposure to fibrils and TNF alpha could impact the survival of dopaminergic neurons in PD, by diminishing the supportive capacity of astrocytes,” explains Dr. Laurent Roybon, co-senior author of the study.
Finally, the researchers report that while astrocytes are able to degrade smaller fibrils, this is not the case for very large aggregates, similar to those observed in the later stages of PD.
“Our findings highlight that when identifying a therapeutic window for future treatments of PD we may have to act as sooner rather than later,” reflects Dr Roybon. “If the processes are too advanced and the aggregates too large then it will not be possible to degrade these structures and reverse the progression of the disease.”
“This study emphasizes the strength of combining expertise, methods and results from different fields to tackle complex phenomena and gain novel insight into processes within the brain and neurological diseases,” concludes Prof. Mauno Vihinen, head of the Protein Bioinformatics group at Lund University and co-author of the study.
The study received support from the Michael J. Fox Foundation, the European Joint program for neurodegeneration, the Swedish research council, as well as the Crafoord, and many other national foundations.